Abstract
Background: Primary effusion lymphoma (PEL) is a rare, B cell non-Hodgkin lymphoma (NHL) caused by Kaposi sarcoma herpesvirus (KSHV), also known as human herpesvirus 8, that is strongly associated with HIV infection. PEL often presents as malignant body cavity effusions but can also present as extracavitary masses. Patients may also have concurrent Kaposi sarcoma (KS) or multicentric Castleman disease (MCD). 80% of PEL is also positive for EBV, and in a cohort of 20 patients we previously showed EBV + PEL had improved overall survival (OS) (Lurain et al. Blood 2019). PEL prognosis is poor compared to other HIV-associated NHL with median survival of 6-10 months. While patients are often treated with chemotherapy regimens used in other NHL, the optimal front-line and subsequent-line treatments are unknown. In this largest cohort of patients with PEL in the United States, we evaluated survival, prognostic markers, and second-line treatments in relapsed/refractory disease.
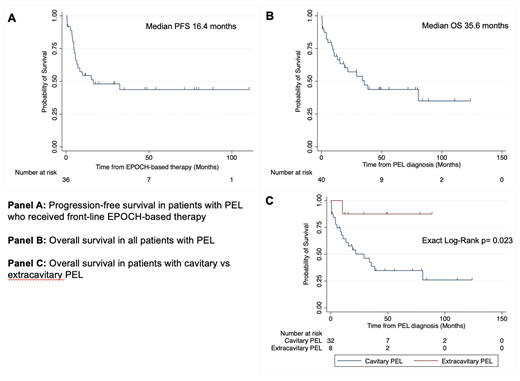
Methods: We analyzed clinical records of all patients with PEL treated in the HIV and AIDS Malignancy Branch at the National Cancer Institute from 2000-2021. We collected demographics, disease characteristics, concurrent KS and MCD, EBV status of tumor by EBER staining, and laboratory data at diagnosis as well as at progression and subsequent lines of therapy. We calculated overall survival (OS) of all patients and progression-free survival (PFS) in those who received front-line EPOCH by Kaplan-Meier method. The survival of extracavitary vs. cavitary PEL was compared using an exact log-rank test. A univariate Cox proportional hazard model was performed to determine prognostic variables associated with OS.
Results: We identified 40 patients with PEL: 38 cisgender men, 2 cisgender women; 18 non-Hispanic Black, 6 Hispanic, 16 non-Hispanic White; median age 41 years. At diagnosis of PEL, 29 patients had concurrent KS, and 7 had concurrent MCD. Eight patients had only extracavitary disease, and 5 had leptomeningeal disease. All but 1 had HIV, and all with HIV received antiretroviral therapy. At diagnosis, median HIV viral load (VL) was 50 (IQR: 27-8323) copies/mL, median CD4 + cell count was 100 (IQR:44-395) cells/µL, and median KSHV VL was 4147 copies/10 6 cells (IQR:178-68,526). One patient died prior to receiving treatment. Of the 39 patients who received front-line treatment, 38 received combination chemotherapy (EPOCH [36], CHOP [1], ICE [1]) with rituximab added in 34 patients to treat concurrent MCD or deplete the KSHV-infected B cell reservoir. One patient received pembrolizumab as up-front therapy due to concurrent progressive multifocal leukoencephalopathy. Twenty-three (57%) had complete remission (CR) by Lugano criteria. Median PFS after front-line EPOCH was 16.4 months (Figure 1a), and median OS in all patients was 35.6 months (Figure 1b), with 5-year OS of 44%. Median OS for patients with extracavitary disease was significantly higher than in patients with cavitary disease (p=0.023, Figure 1c). EBER-positive tumors (HR=0.21, p=0.005) were associated with improved survival, while concurrent KS, MCD, leptomeningeal disease, and baseline CD4 and KSHV VL were not associated with OS outcomes.
Eleven patients with relapsed/refractory disease received second-line therapy, including combination chemotherapy (3); brentuximab (3); pembrolizumab (1); pembrolizumab and pomalidomide (1); interferon-alpha, ganciclovir, and bevacizumab (1); bortezomib, ganciclovir, and zidovudine (1); and radiation to pelvic lymph nodes (1). Five of these patients received subsequent treatment after disease progression, including 2 patients with leptomeningeal PEL, 1 who received daratumumab and 1 who received pomalidomide and pembrolizumab with ongoing CRs at 12 months and 33 months, respectively.
Conclusion: Patients with PEL had a median OS of 35.6 months, which is improved from previous reports. Patients with extracavitary PEL appear to have improved OS, and we confirmed our prior study noting EBER-positive PEL is a positive prognostic marker. Promising chemotherapy-sparing treatment regimens in relapsed/refractory PEL, include pembrolizumab, pomalidomide, and daratumumab.
Uldrick: Regeneron: Current Employment; Roche: Research Funding; Merck: Other: Receives study drug; Celgene: Research Funding. Yarchoan: Celgene: Research Funding; Merck: Other: Clinical Trial Support; EMD-Serano: Other: Clinical Trial Support; Eli Lilly: Other: Clinical Trial Support; CTI BioPharma: Other: Clinical Trial Support; Janssen Pharmaceuticals: Other: Clinical Trial Support; U.S. Dept of Health and Human Services: Patents & Royalties. Lurain: EMD-Serrono: Research Funding; BMS-Celgene: Research Funding; CTI Biopharma: Research Funding; Merck: Research Funding; Janssen: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal